1-month-old baby health & growth guide
It’s been one whole month since your baby was born, mama. Looking back, does it feel like ages ago or just yesterday? (It might be a combination of both.) You and your little one have already grown in so many ways—truly blossoming together—but know that you may still be figuring each other out, too. Here’s what you can expect regarding 1-month-old baby weight and growth, plus tips for care, sleep and feeding.
Related: 1-month-old baby milestones
1-month-old baby nutrition
When it comes to feeding a 1-month-old, aim to follow your baby’s hunger cues—like rooting, turning their head from side to side or crying—which is known as the responsive feeding method. No strict schedules just yet.
Feeding
It might feel like your lovebug is hungry all the time—and that’s because, well, they are. Though baby’s stomach is still small, it’s growing every day.
According to The American Academy of Pediatrics and La Leche League, at 1 month old, babies should be consuming the following amounts at the suggested times below, but remember to follow your baby’s hunger cues.
How much to feed a 1-month-old baby
Breast milk: 2 to 3 ounces every 2 to 3 hours
Formula: 2 to 3 ounces every 3 to 4 hours
Take note that your baby’s feeding windows may be a bit more spread out if you’re offering formula, as formula tends to be digested and metabolized more slowly than breast milk.
Related: Four-week-old baby feeding schedule & amounts
Common feeding issues: What to know about colic
You might have heard the term “colic” being tossed around a lot in your baby’s newborn phase. Here’s what it means: Colic is a term for when an otherwise healthy baby cries a lot for no clearly understood reason. Colic is diagnosed by the 3/3/3 rule: When an infant under 3 months of age cries for more than three hours, more than three days a week. Colic may contribute to feeding issues in babies.
Doctors don’t truly know what causes colic: It could be related to a sensitivity to some component of breast milk or formula, but they do know it’s not caused by gassiness. Some colicky babies also have gas due to the amount of air they swallow when crying—but it’s not gas that’s causing the colic. (Read more about gas below.)
Colic could also be related to overstimulation, a baby’s inability to calm themselves or sensitivity to the sights and sounds of their environment. The good news? Colic typically goes away by the time a baby is 3 or 4 months old.
Talk to your baby’s pediatrician if you feel like your little one is crying nonstop or seems inconsolable, especially later in the day or evening hours. They might recommend a gentle elimination diet if you’re breastfeeding, a formula change, or probiotic drops.
Related: Probiotics may be the answer to soothing your baby’s colic
1-month-old baby weight
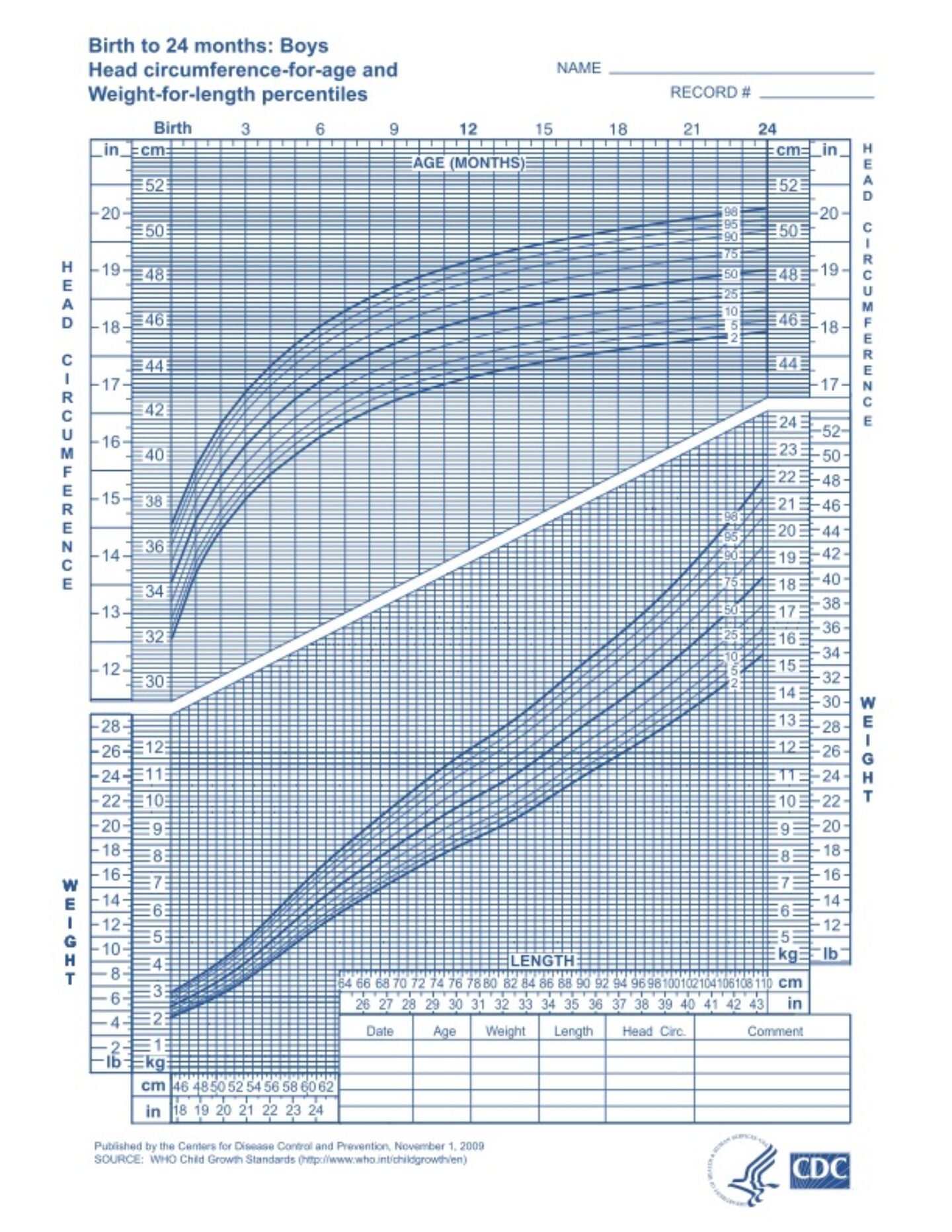
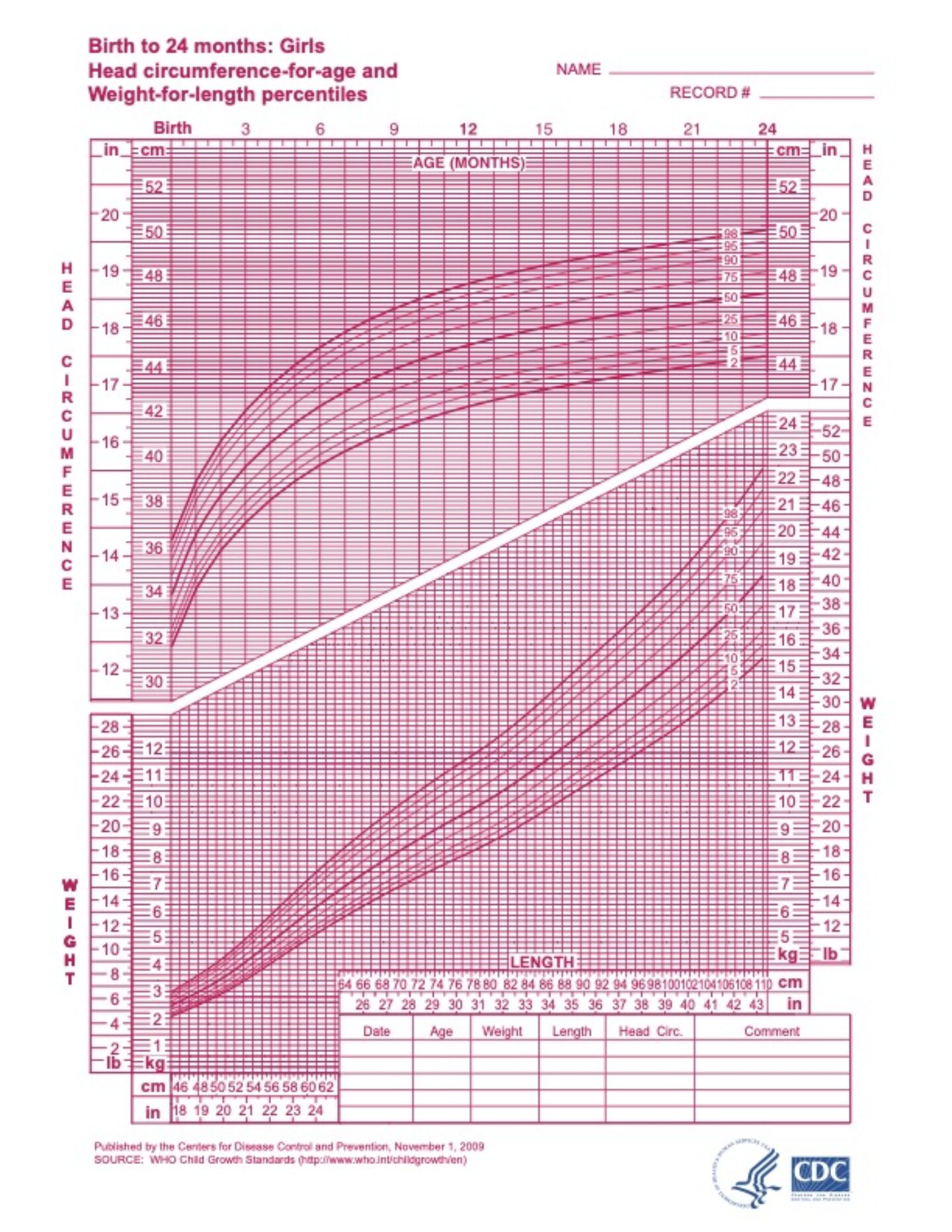
For babies up to 2 years of age, the Centers for Disease Control and Prevention (CDC) recommend using the World Health Organization (WHO) weight and length charts.
The WHO growth charts for babies 0 to 2 years are based on what is standard for a predominantly breastfed infant. According to the organization, the WHO charts reflect growth patterns among children who were predominantly breastfed for at least 4 months and were still breastfeeding at 12 months. The American Academy of Pediatrics (AAP) recommends continuing to breastfeed for at least two years, as long as it benefits both mother and baby.
How much does the average 2-month-old weigh?
According to the WHO:
- A 2-month-old baby boy in the 50th percentile weighs 9 pounds, 14 ounces (4.5 kilograms)
- A 2-month-old baby girl in the 50th percentile weighs 9 pounds, 4 ounces (4.2 kilograms)
What factors contribute to a 1-month-old baby’s weight?
You might be hyper-focused on your newborn’s weight in their first month, as babies typically lose 7% to 10% of their birth weight in the first week of life. Growth-wise, the first two weeks of life are focused on gaining that weight back, and then some. During the first month, most newborns gain around 1 ounce of weight per day.
Your pediatrician will review your baby’s weight with you at your 1-week and 1-month well visits, and they can let you know if your little one is on the right track. Try not to stress—if your doctor is worried about how things are going, they’ll let you know.
There are several factors that contribute to how much your baby weighs in month one, including:
Size at birth: The weight of your baby at birth will influence their weight in the first month.
Assigned sex at birth: Males tend to weigh a bit more than females, and tend to gain weight slightly faster.
Gestational age: Babies born preterm or early full term may weigh less than babies born full or late-term.
How they’re fed: Breastfed babies may gain weight slightly faster than formula-fed babies in the first 6 months of life, according to AAP.
1-month-old baby length
Between birth and 6 months, babies grow an average of 0.5 to 1 inch each month. From 7 months to 12 months, babies are more likely to grow an average of ⅜ inch each month.
How long is the average 1-month-old?
According to the WHO:
- A 1-month-old baby boy in the 50th percentile is 21.5 inches long (54.7 cm)
- A 1-month-old baby girl in the 50th percentile is 19.4 inches long (49.15 cm)
What factors contribute to a 1-month-old baby’s length?
There are several factors that contribute to your baby’s length in month one, including:
Genetics: The height of a baby’s parents and other family members strongly influences their future height.
Assigned sex at birth: Males tend to be slightly taller than females.
Nutrition: Complete nutrition during pregnancy and after birth can contribute to future growth.
Sleep duration: One study has shown that infants grow in length after long naps.
Growth charts and percentiles
Growth charts are used by pediatricians and other health practitioners to track a baby and child’s growth as they get older. They show how a baby’s weight or length may be compared to the weight or length of other babies of the same age.
For example, if a baby’s weight is in the 40th percentile, it means that 60% of babies of the same age and sex weigh more, and 40% of babies weigh less. Your pediatrician will plot your child’s growth on their chart at each well check, and look at the overall curve for trends.
While your little one’s growth is a good indicator of their overall health, it’s important to remember that growth charts are just one tool used to track a child’s development (along with developmental milestones and their feeding habits) and aren’t meant to be used alone.
Growth spurts
On average, babies grow the fastest in the first 6 months of life—upwards of 4 to 7 ounces per day in weight, and around 1 inch per month in length. Growth slows down a bit between months 7 and 12. While weight and length gain may be steady for several months, growth isn’t always linear throughout the first year. A growth spurt might slightly change the growth pattern on your child’s growth chart; jumping your little one to a different weight or length percentile.
Doctors look at the shape of the overall curve on the growth chart—what’s known as the growth pattern. Not as much attention is focused on the month-to-month changes; it’s about the overall picture.
In the first month of life, baby growth spurts tend to happen around days 10 to 14, and may last up to a week.
Growth spurts can mean your baby might be a little fussier or a little (or a lot!) hungrier. It’s not uncommon to see more cluster feeding and more night wakings around the time of a growth spurt. Your little one needs to take in more energy to support their growth—and may require more cuddling, too.
When should I worry about my baby’s growth?
Your baby’s growth should generally be following a consistent curve. Try not to stress too much: While your 1-month-old baby’s weight is one metric of how well they’re developing, it’s not the only one. Head circumference and length also play a role, as well as developmental milestones.
According Boston Children’s Hospital, signs of slow growth in babies may include the following:
- If your baby doesn’t regain their birth weight in the first 14 days after birth
- If your newborn up to 3 months isn’t gaining around an ounce a day
- If your baby has been growing steadily and suddenly stops growing
If you’re concerned, reach out to your child’s pediatrician. They’ll examine how frequently your little one is feeding, how much they’re taking in at each feed, and the number of wet and dirty diapers to try to get the full picture.
Related: How many newborn diapers do you need? The answer may surprise you
1-month-old baby sleep
Your newborn will still be sleeping most of the time throughout their first month. Keep in mind that your 1-month-old’s sleep shouldn’t follow a true schedule just yet. Keep focusing on their sleepy cues (more on those below), which will help prevent them from getting overtired. And if you’re holding them for naps (aka contact napping)? That’s definitely OK.
Baby sleep cues to look out for:
- Staring off into space or a glazed-over look
- Looking away
- Flushed or slightly reddened brows
- Big yawns
- Rubbing eyes
- Fussiness
What baby sleep looks like at 1 month:
- Your baby may be taking 4 to 5 naps per day
- Your baby may be sleeping in 2- to 4-hour windows at night
- Your baby may be awake for 30 minutes to 45 minutes at a time
Read more: How much sleep does a 4-week-old baby need?
Diapering a 1-month old
Taking stock of your newborn’s stool can be a helpful way to know if they’re getting enough milk and can help you spot signs of dehydration or constipation.
What to know about poop
Another (somewhat messier) metric of your child’s growth and development is their diaper output. Yep, your baby’s poop can hold clues to their health. The key factor is figuring out what’s considered “normal” for your infant, as all babies are different, and poop output may depend on how they’re fed. It’s then the big variations that may signal that something is off, like if your baby dirties 4 diapers a day and then suddenly doesn’t poop for a whole day that may warrant a check-in with the pediatrician.
Poop in breastfed babies
Texture: Breastfed babies tend to have more frequent, softer poops. Stool may be somewhat seedy and liquidy.
Color: After birth, your baby’s first bowel movements were probably a tarry black color, known as meconium. Once a baby starts consuming breast milk, their poop may be more greenish in hue. After the first week, in an exclusively breastfed baby, poop may be a yellow mustard color.
Frequency: Breastfed babies may poop anywhere from 3 to 7 times per day in the first month, but there may also be days where an infant doesn’t poop. AAP states that if your exclusively breastfed infant is pooping less than once per day, it could mean they’re not taking in enough breast milk. “However, breastfed infants may go several days or even a week between bowel movements, using every drop they eat to make more baby, not poop,” notes AAP.
Poop in formula-fed babies
Texture: Formula-fed babies tend to have firmer bowel movements, usually the consistency of paste or peanut butter.
Color: Stool color may be tan, yellow or greenish.
Frequency: Formula-fed babies may poop anywhere from 1 to 4 times per day in the first month. AAP reports that formula-fed babies usually poop at least once per day, but may go 1 to 2 days without pooping.
Related: 30 stylish diaper bags that don’t look like diaper bags
Coterie
• $90The Diaper – 1 Month Supply
Coterie has upgraded basically every aspect of diapering. Their plush, cashmere-like disposable diapers absorb moisture super fast to prevent not only leaks, but rash and redness as well. The eco-friendly design is also free of fragrance, lotion, latex, rubber, dyes, alcohol, heavy metals, parabens, phthalates, chlorine bleaching, VOCs, and optical brighteners. Your baby’s bottom deserves the best–and these are pretty perfect.
Aquaphor
• $15.97Baby Healing Ointment
Aquaphor is the stuff of dreams—from chapped lips to minor cuts + scrapes, there’s hardly anything that this magical ointment can’t help with. And diaper rash is no exception!
Aquaphor protects baby’s skin from wetness, acidity and chafing, and unlike petroleum jelly, creates a barrier over the skin which heals while still enabling the flow of water and air. Added bonus—it also works great on mama’s dry hands!
Ubbi
• $69.99Steel Odor-Locking Diaper Pail
The Ubbi diaper pail costs more than others upfront, but you don’t have to buy special bags if you don’t want to. That’s right—this one works with regular bags just fine (and still blocks odor!) A winner of nine awards proving that parents everywhere love it, the Ubbi pail is different in that it’s made from steel, which is not porous like plastic, so the pail truly traps in odor. And it comes in 15 different colors, so you can find one that fits your nursery decor.
Common concerns
Constipation and gas in 1-month-old babies are the most common concerns when it comes to baby poop. Remember that there’s a wide range of normal in these early days and weeks, but if you have any questions, reach out to your child’s pediatrician.
Constipation in 1-month-olds
If your newborn is passing hard, dry stools, they could be constipated. Many babies tend to look like they’re straining when having a bowel movement, and a cry or going red in the face is all within the realm of normal (it’s hard to poop laying down!).
According to AAP, signs of infant constipation may include:
- Straining for more than 10 minutes
- More frequent spitting up
- Excessive fussiness
- Fewer bowel movements
- Unusually hard stools, or passing stools with dried blood
If your little one is showing signs of constipation, reach out to your pediatrician. They might recommend the following remedies, but be sure to check in with them first.
1-month old baby constipation remedies
If your infant is over 1 month old, you can try offering them a little apple juice or pear juice. Juice isn’t typically recommended for babies under 1 year, but the sugars in these fruit juices help draw liquid into the intestines and can be helpful for constipation, AAP notes.
Try offering 1 ounce a day for every month of life up to about 4 months (a 1-month-old baby would get 1 ounce) until symptoms resolve.
Gas in 1-month-olds
All food is new food to an infant, whether that’s breast milk or formula, and gas is a normal part of their digestive process. It can cause some discomfort, however, so taking steps to reduce gas can be helpful in preventing future fussiness.
Here are a few ways to prevent and relieve gas:
How to prevent and relieve gas in a 1-month-old baby
- Increase tummy time and movement
- Burp after feedings
- Ensure a good latch on both breast and bottle
- Try infant massage and bicycle legs
- Using a more upright posture when feeding
- Opting for ready-to-use liquid formula rather than powdered formula
A note on diet and breastfeeding
There’s no real evidence that certain foods cause more gas in babies than others, which means that yes, you can keep eating broccoli. If your baby has a true sensitivity to certain food groups, such as dairy, you may notice other symptoms, such as more spitting up, excessive fussiness, rash, diarrhea or other changes. In those cases, your physician may recommend you eliminate dairy (dairy, eggs and peanuts are the most common causes of food allergies in babies) for two weeks to see if symptoms improve.
Ask your pediatrician about baby probiotics, too, which may help with digestive discomfort.
TruBiotics
• $17.99Baby Digestive + Immune Health Soothing Probiotics Drops with BB-12
These soothing drops are made from high oleic sunflower oil to help support baby’s digestive and immune health. One of the most clinically studied probiotic strains, BB-12 has been shown to reduce crying and fussiness associated with colic.
Culturelle
• $23.99Baby Grow + Thrive Probiotics + Vitamin D Drops
Complete with clinically studied probiotic strains BB-12, Lactobacillus rhamnosus GG and vitamin D, Culturelle’s Baby Grow + Thrive formula has everything your little one needs, whether they’re breastfed or formula-fed.
Caring for a 1-month-old
It might feel like there’s a steep learning curve when it comes to caring for your baby—but know that between the challenging moments (like diaper fails and baby colds) there are so many sweet ones, too (first smiles and all the snuggles). Here’s what to know.
Related: Your 10 most pressing baby safety questions, answered by a pediatrician
Baths
Bathtime can be a lovely way to connect with your 1-month-old. You don’t need to bathe them daily—as a rule of thumb, AAP recommends a bath three times a week for babies younger than 12 months. Also know that for babies under 6 months, no soap is necessary, Neela Sethi, MD, a MAM Baby ambassador and practicing pediatrician, tells Motherly. Clean, warm water is all you need until they start crawling around and truly getting dirty.
Related: How to give an infant a bath, in 5 simple steps
Before your newborn’s umbilical cord falls off, stick with sponge baths. Once the umbilical area is healed, you can try a lukewarm water bath. Water should be warm but not hot—you can test it using the inside of your wrist or elbow.
Aim to make baths should be brief, around 5 to 10 minutes, and try to wash their hair last (so they don’t get too cold). Be sure to have all your supplies at the ready (towel, washcloth) so that you never leave baby unattended, which is a big drowning risk.
Related: 14 bath safety tips for babies and kids of all ages
Angelcare
• $19.78Baby Bath Support
With a solid 5-star rating, Angelcare Baby Bath Support is a top choice for taking the stress out of newborn baths. It’s not a tub, instead, it offers a safe and comfortable place for your baby to lounge in the sink or regular bathtub. The ergonomic design keeps them at an incline without submerging them too much and is made from a soft mildew-resistant mesh that’s gentle on their skin. Without any nooks or crannies for mold to grow in it’s super easy to keep clean and can hang for storage when not in use.
Mustela
• $18.50Gentle Cleansing Gel
Safe and effective without stripping baby skin of its natural oils, Mustela’s Gentle Cleansing Gel is fortified with Vitamin B5 and Avocado Perseose, a patented natural ingredient specifically designed to help protect and hydrate dry skin.
Nails
Those newborn nails may seem soft, but they can be surprisingly sharp. That’s where baby mittens can come in handy (pun intended), though AAP notes it’s best to use them at night to allow baby plenty of time to explore their hands during the day. Once babies turn 1 month old, those tiny nails start to harden and you might be able to trim any sharp edges to prevent future scratches.
How to trim baby’s nails:
- Using baby nail clippers, or small clippers with rounded edges, gently push down the finger pad to reveal the nail edge, and then trim the edge along the natural curve of their nail. You can file off any sharp corners with an emery board.
- For toes, clip straight across.
- Be careful not to get too close to the quick.
A pro tip: Trim nails while your little one naps, if you can catch them when they’re in a deep sleep (there’s less chance of them pulling away). Or, loop in a helper to keep baby steady while you work.
Frida Baby
• $12.99NailFrida The SnipperClipper Set
These easy-to-use nail clippers are specifically designed for teensy baby nails and feature a helpful spy hole so you know where you’re clipping. The set also includes a curved file to buff away those microscopic but oh-so-sharp edges.
Burt's Bees
• $12.95Organic Cotton Baby Mittens
Made with earth and baby-friendly organic cotton, these simple mittens are lightweight and machine-washable.
Common concerns
From cradle cap to baby’s first cold, here’s how to know when you can handle things at home versus when to call the pediatrician.
Cradle cap
Around 3 to 4 weeks after birth, your baby’s beautiful head might show signs of redness or scaly, flaky skin. Cradle cap, or seborrheic dermatitis, is a highly common, non-contagious skin condition that may be a result of an overproduction of oil related to hormonal changes. Doctors aren’t really sure why it happens, but we do know that it’s unlikely to be uncomfortable or itchy for your infant. It’s not related to an allergy or hygiene issue. Cradle cap tends to go away on its own in a few weeks to months, but it can be tough to just watch and wait.
In some cases, seborrheic dermatitis can also be found on the face and groin, too. If this is the case, reach out to your pediatrician for tips.
How to manage cradle cap
Cradle cap can be managed at home if it’s confined to your baby’s scalp, AAP says.
- Aim for frequent shampooing. Using a soft baby shampoo a few times per week and brushing with a soft brush can help remove the scales.
- Petroleum jelly applied to the scales may help keep things moisturized, but avoid baby oil or mineral oil, which can cause more buildup.
- If it seems severe, talk to your doctor to see if a cortisone cream is warranted.
Tubby Todd
• $49Bye Bye Cradle Cap Bundle
A one stop shop to banish cradle cap! This well crafted kit includes hair + body wash, all over ointment and Tubby Todd’s effective (and plant-based!) Bye-Bye Cradle Cap gel which is formulated with Zinc Pyrithione to help soothe and reduce flaking, scaling, redness and other symptoms of Cradle Cap. Use with the included soft, antimicrobial silicone brush to gently buff away flakes post bath time for a clear and healthy scalp.
FridaBaby
• $13.49DermaFrida The FlakeFixer
This 3-step cradle cap system features a sponge for lathering up, a soft bristle brush to loosen flakes and a super fine comb to lift it all away–all neatly packed on its own little stand!
Baby acne
If you thought only pubescent teenagers got acne, think again. Baby acne is a normal occurrence in the first two months of life (so cruel!), and consists of tiny pimples that arise due to stimulation of the oil glands in the skin by hormones passed via the placenta during pregnancy.
How to manage baby acne
AAP recommends gently washing baby’s face once a day with mild baby soap to remove milk residue, and opting for gentle detergents when laundering sheets and burp cloths. Harsh detergents can irritate their sensitive skin further.
Related: Answers to questions about baby skin woes—from a pediatric dermatologist
Mustela
• $17No Rinse Cleansing Water
Perfect for in between baths, this gentle micellar water cleans your baby’s face, body, and diaper area while softening the skin.
Illness
Your baby’s first cold is a milestone no parent is rushing to reach. It’s always hard when your little one is sick, and it’s even tougher when it happens in the first month. But most kids will have 8 to 10 colds before they turn 2 years old, AAP notes. And most come and go without any problems.
But babies’ immune systems are still developing, so it’s important to watch for signs of high fever or viruses that can impact breathing, like RSV. If you have any concerns, it’s always encouraged to reach out to your child’s pediatrician. Here’s what to know about baby illness.
How to manage baby illness and when to see a doctor
- Fever: If your child is under 3 months and spikes a fever, call your pediatrician for guidance. They may recommend coming in for a visit or offering acetaminophen—but they’ll have to give you correct dosing information.
- Congestion: If your little one has a congested nose, it can make feeding more difficult, so you may need to increase the frequency of feeds (just offer smaller amounts at each one). Saline nasal sprays can also and running humidifiers can also make it easier for tiny noses to breathe.
- Vomiting: Babies spit up a lot, but if it’s true vomiting, it’ll be a forceful reflex and will likely coincide with some tears. Reach out to your child’s pediatrician to try and identify the cause.
Related: 12 must-have products for baby’s first cold
Kinsa
• $24.98Smart Thermometer
We know that fevers (especially baby’s first fever) can be incredibly scary for everyone, but let’s take a deep breath and remember: fever is the body’s natural response to infection. It’s definitely not fun, but generally no cause for worry. That said, always reach out to your child’s pediatrician with questions or if something feels off to you. (We love the Parents’ Guide to Fevers infographic from the Cleveland Clinic for a quick and easy reference for all things fever, btw.)
Now that that’s out of the way… you’re going to need an accurate way to take baby’s temperature. Ear, forehead, and oral thermometers are great for older kiddos, but for little ones under a year, a rectal thermometer is the best and most accurate choice. (Momlife is endlessly glamorous, isn’t it?)
We’re smitten with this digital, smartphone-compatible option—it’s accurate + easy to use, FDA-cleared, affordable, and best of all keeps a record of its readouts and offers guidance on what to do next. (And when they’re older and more reluctant, the app includes a bubble game and Sesame Street mode to keep them happily distracted.)
Munchkin
• $7.23The Medicator
The medicator dispenses liquid medicine at a safe flow rate for baby that minimizes choking and coughing. The design bypasses taste buds so the chances of spitting are lessened for medicine that goes down easily. It also comes in a variety of colors, so you’re sure to find something that pleases your picky toddler.
FridaBaby
• $19.86NoseFrida
We’d love it if every infant came equipped with the ability to blow their own nose, but alas, that duty is still left up to us. When your little one has the sniffles, ditch the outdated bulb syringe and opt for the award-winning NoseFrida, proudly referred to as The Snotsucker. The mechanics seem a little gross at first (yes, you are actually sucking the snot out of that little nose!), but trust us, it’s worth it.
A note from Motherly on self-care while caring for a 1-month-old
The days spent caring for an infant may feel long, but mama, we know they can feel even more endless if you don’t take a few moments for yourself. If you find yourself struggling to enjoy the things you used to love, having a hard time adjusting to your new life or role or feeling isolated or lonely, help is out there. Postpartum depression (PPD) and related conditions can set in anytime in the first year after birth. Your mental health is always a priority—reach out to a loved one to help you connect to the resources below.
Postpartum depression resources
If you’re experiencing any postpartum mood symptoms, no matter how mild, know that help is available. Reach out to your healthcare provider about next steps and potential treatment options, such as more support at home, therapy or medication. If you’re in crisis, reach out to a crisis hotline or dial 988 or 911 for immediate support.
The phone numbers listed below are available to you 24/7 to help you with suicidal thoughts or other mental health crises.
-
The National Maternal Mental Health Hotline: 1-833-943-5746 (1-833-9-HELP4MOMS)
- Available in English and Spanish and in a completely confidential line.
-
Postpartum Support International: 1-800-944-4773 (call or text)
- Available in English and Spanish
- National Crisis Text Line: Text HOME to 741741
-
National Suicide Prevention Hotline: Call or text 988
- Available in English and Spanish
